This is a 6-minute read.
Breast cancer-related lymphedema (BCRL) is a chronic condition and a common consequence of breast cancer treatment. It’s a significant concern in the United States, where 1 in 8 women will develop breast cancer during their lifetime.
A study published in the journal Cancer reports that the overall prevalence of BCRL is 6.8% at baseline after cancer diagnosis. This figure rises to 19.9% at two years post-diagnosis and 23.8% at seven years post-diagnosis. Between 88% and 93% of patients develop lymphedema in the arm, and 14% to 27% have it in the trunk or breast.
While BCRL is often called “post-mastectomy lymphedema,” this is a misnomer. Cancer-related lymphedema can also occur after radiation therapy or surgical treatments conserving part or all of the breast.
Common Breast Cancer-Related Lymphedema Symptoms
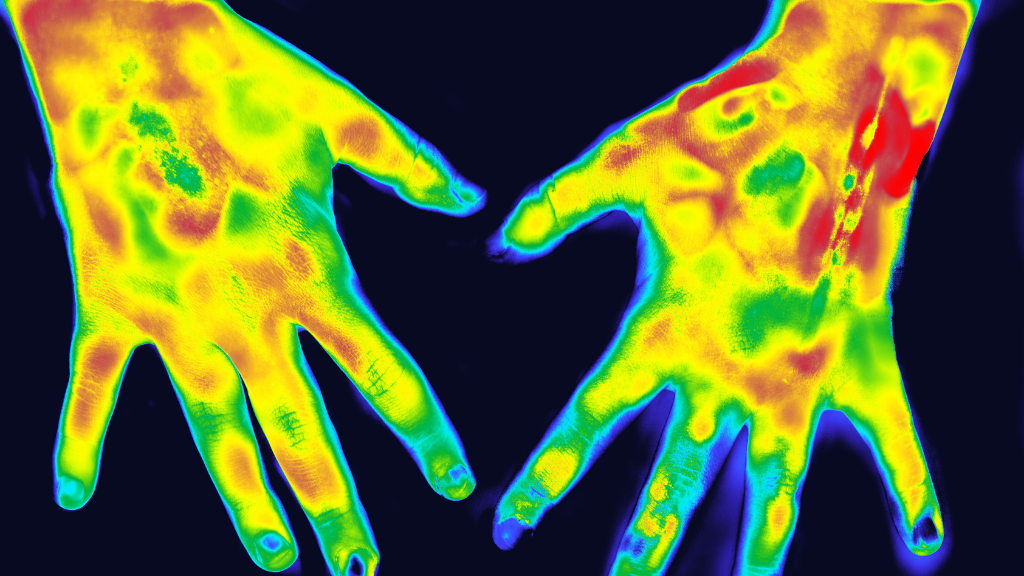
The first symptoms of BCRL are usually swelling, tightness, numbness, tingling, or pain in the shoulder area. The swelling of BCRL often manifests in the arm, hand, breast, or chest wall on the side where lymph nodes were removed or damaged during surgery or radiation therapy.
Persistent truncal swelling may occur in BCRL and can cause significant disfigurement and disability. While each case is unique, this may include pain, motion-limiting fibrosis, axilla (underarm) swelling and cording, and progressive enlargement of the breast.
Often, the thorax is overlooked by physicians and other clinicians. Historically, BCRL was recognized as arm swelling with less attention paid to the truncal region. Other patients report feeling uncomfortable with discussing the breast region as well, thus limiting attention to this affected area.
However, consistent therapy and self-care can help manage and reduce the symptoms of BCRL regardless of its location in the body. Treatments may include some or all of the following:
- Manual lymphatic drainage (MLD), a specialized massage technique for lymphatic fluid movement
- Multi-layer short stretch compression bandaging
- Compression garments
- Pneumatic compression pumps
- Exercises to promote lymph flow
- Skin care to prevent infections
Using the Lympha Press® Optimal Plus to Treat Breast Cancer-Related Lymphedema
The Lympha Press® Optimal Plus with ComfySleeve™ pneumatic compression therapy garment is clinically proven to effectively support management of BCRL symptoms. The ComfySleeve™ half jacket is specifically designed for effectiveness and ease of use.
This innovative device treats the arm, shoulder, chest, back, and abdomen using the principles of manual lymph drainage (MLD). Multiple chambers and a patented Pretherapy™ treatment mode prepare the body for proximal decongestion and apply targeted pneumatic compression as needed.
A dedicated chamber gently compresses the ipsilateral axilla for excellent decongestion of the underarm and shoulder area. The garmet’s fill-to-fit design includes thoughtfully-placed zippers and a side-release mechanism, allowing a patient to use either hand to easily apply and remove the garment.
Overlapping chambers create directional lymph flow without gaps, and the device comes with calibrated gradient compression and fully adjustable pressure. Choose from sequential or wave decongestive modes for optimal therapy customization and use an Android, iPhone, or tablet-based app to configure therapy options.
Proven Effectiveness for treatment of Breast Cancer-Related Lymphedema
Advanced pneumatic compression using Lympha Press has been clinically supported to stimulate lymphatic uptake and transport in lymphedema patients1. Specifically in studies of breast cancer related lymphedema patients, Lympha Press treatment has been shown to reduce tissue stiffness2, reduce swelling3 and, when used together with techniques of MLD, decrease pain and increase shoulder range of motion4.
A multi-case report of lumpectomy patients who experienced severe thoracic radiation damage with significant persistent symptoms, including thoracic pain, swelling, and fibrosis, after conservative therapy (manual lymph drainage, compression, elevation, exercise, and skin care) indicated these patients experienced positive outcomes following treatment in-clinic and self-administered therapy at home with the Lympha Press® Optimal Plus pneumatic compression therapy system using the ComfySleeve™ 1-75 half jacket garment. These positive outcomes include reduced swelling and pain and increased range of motion.
After four weeks of at-home treatment, patients had decreased arm and thoracic swelling, decreased pain, and increased functional range of motion of the arm, along with significant relief of pain, hardness, and tightness in the breast. The final measurements in this study demonstrated a carryover effect of decongestion for up to three days following Lympha Press treatment.
Subjective pain experience also decreased dramatically for those Lympha Press users. Most importantly, participants reported that their breasts no longer felt hard or tight, with one patient even able to use a breast prosthesis after her edematous breast was reduced.
Key Takeaways for BCRL Treatment
With a significant rate of global breast cancer incidence and related lymphedema, effective treatments can make a notable difference for millions of individuals. Healthcare professionals and their patients deserve treatments that offer evidence-based effectiveness, including The Lympha Press® Optimal Plus.
To learn more about treating lymphedema, find a number of resources and support from the Lympha Press community. For more information about acquiring treatment devices backed by clinical studies to treat BCRL, please contact us.
References
1. Aldrich MB, Gross D, Morrow JR, Fife CE, Rasmussen JC. (2017) Effect of pneumatic compression therapy on lymph movement in lymphedema-affected extremities, as assessed by near-infrared fluorescence lymphatic imaging. J lnnov Opt Health Sci. Mar;10(2):1650049.
2. Bok SK, Jeon Y, Lee JA, Ahn SY . Evaluation of Stiffness in Postmastectomy Lymphedema Using Acoustic Radiation Force Impulse Imaging: A Prospective Randomized Controlled Study for Identifying the Optimal Pneumatic Compression Pressure to Reduce Stiffness. Lymphat Res Biol. 2018 Feb;16(1):36-42.
3. Johansson K, Lie E, Ekdahl C, Lindfeldt J. A randomized study comparing manual lymph drainage with sequential pneumatic compression for treatment of postoperative arm lymphedema. Lymphology. 1998 Jun;31(2):56-64
4. Avrahami R, Gabbay E, Bsharah B, Haddad M, Koren A, Dahn J, Zelikovsky A. Severe lymphedema of the arm as a potential cause of shoulder trauma. Lymphology. 2004 Dec;37(4):202-5.