This is an 18-minute read.
In February 2023, Lympha Press hosted a webinar about infrared thermography for lymphedema and wound care presented by Frank Aviles, Jr., PT, CWS, FACCWS, CLT-LANA, ALM, AWCC, DAPWCA. The webinar is part of the Lympha Press Education Series on YouTube, focusing on evidence-based research into lymphedema treatment.
The following article provides an overview of the webinar. It starts with a look at the connection between conducting a visual clinical inspection of the skin and using thermographic imaging. Next, we’ll outline helpful tools for clinical judgment. Finally, we’ll wrap up with examples from Aviles showing notable differences between visual examination and thermographic imaging.
Starting at the Skin Level
The skin often shows what’s happening deeper within the body. Each layer has a function, and blood must reach the skin to nourish it. When the nourishing blood flow is absent, the skin will show the signs. A visual assessment, however, may not be enough to tell the whole story.
Aviles explains that a visual examination might indicate that a patient has cellulitis, but it might instead be acute lipodermatosclerosis, which mimics hepatitis. A lymphedema patient may have signs of infection or dermatitis. Someone with an open wound may have signs of dehiscence or infection.
Visual assessments are sometimes more challenging when people have darker skin. For example, darker-skinned individuals may have historically been less frequently diagnosed with certain skin problems. This includes patients who live in nursing homes with primarily African American populations, where there are higher rates of pressure injuries.
These patients deserve more thorough forms of assessments. New research is addressing important emerging issues in wound treatment. Thermographic technology doesn’t discriminate based on surface melanin content and can show what’s happening below the skin level.
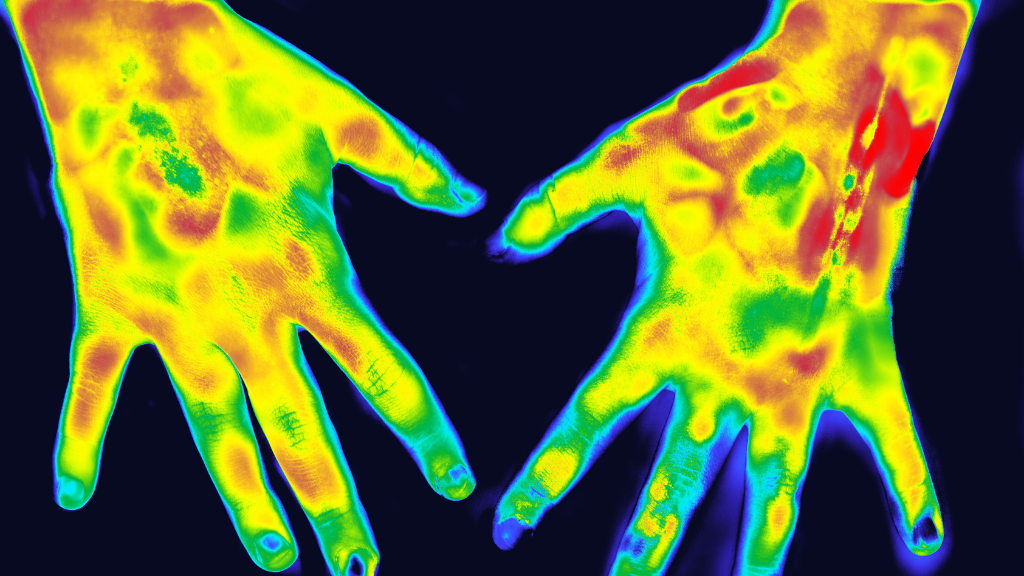
Aviles notes that thermographic images can show the early stages of inflammatory processes. In terms of blood flow, the imaging may highlight ischemia and the potential for infection and inflammation. A patient may show signs of vasculitis when imaged with thermography.
When examining these images, think through diagnostic questions about inflammation and skin tone. For example, a patient with darker skin might have an abscess that has previously been deemed normal skin, but the imaging shows abnormal inflammation under the surface.
Aviles relates that one of his patients had a similar situation, where thermographic imaging showed the patient’s toes were so inflamed that it was quite likely that an infection was brewing. This wouldn’t have been apparent from the patient’s history or etiology.
Another patient in the same clinic had a scalp wound that healed but later became an open wound again. When Aviles was asked to determine the problem, his thermographic imaging lit up in a certain area of the patient’s head. Upon questioning, the patient revealed that he’d recently hit his head on an object, so perhaps he wasn’t getting enough blood flow to that area.
About Thermographic Imaging Technology
Aviles clarifies that thermographic imaging isn’t necessarily diagnostic technology. When he first encountered the technology, it was being used for preventive care. Thermography doesn’t show what is physically located under the top layer of skin. Instead, it gives clues about oxygenation, perfusion, diffusion, and so forth. It provides a new perspective on wound progress.
The technology can also provide a better understanding of what’s going on at the cellular level. It can show whether the metabolic activity is happening normally and what may be happening with the mitochondria and cellular respiration.
Consider acute inflammation. This is a normal healing process of venous insufficiency, lymphedema, and other conditions. Thermography provides clues about chronic inflammation, allowing doctors to stay on the lookout for other symptoms like cold feet, which can indicate ischemia or vascular problems, or hot feet, which might be connected to infection.
Aviles references M. Patel’s 2019 studies showing the lack of criteria to determine cellulitis. According to Patel’s study, 31% of patients going into the emergency room were misdiagnosed with cellulitis. The lymphedema population often has dermatitis and, after a misdiagnosis of cellulitis, may be improperly prescribed antibiotics. Patel revealed that there was no good way to reliably diagnose cellulitis.
Laser thermometry brings new insights, including the widely accepted four-degree difference between extremities, which indicates abnormal inflammation.
It’s even possible to determine whether a patient with diabetes is likely to experience an open wound. Aviles explains that a study by Dr. Javier Ena found that if there was a four-degree difference in temperature between limbs and the patient offloaded with rest, only 8% of participants proceeded to an ulcer. Meanwhile, 23% of the other group, which was not offloading with that degree of difference, ended up with sores.
Aviles says, “All that work led me to think, ‘If thermography can be more precise, why can’t I do the same thing?’”
Thermography has been around since the late 1950s, and today, there are more than 800 studies related to it. Some thermographic machines are FDA-approved, and others are not. The FDA declared that thermography is not a standalone tool and needs to be used with mammograms in the case of breast cancer screening. Yet, one doctor created 18,000 breast cancer thermography images in seven days with images as clear as mammography.
In long-wave infrared thermography, Aviles explains he’s looking at the radiation or thermal energy produced by the body due to improper metabolic activity or abnormal physiological response. Rather than looking at the depth, this type of imaging looks at the intensity of radiation.
Infrared is the wave spectrum the eye cannot see, so the device displays an otherwise invisible light spectrum. Invisible radiation becomes a temperature gradient, providing helpful information about what’s happening at the metabolic level.
Neither of these is a diagnostic tool, Aviles clarifies, but rather a complimentary device to aid the clinician in validating their assessment or interventions and to guide treatments.
Tools for Clinical Judgment
Long-wave infrared thermography uses a non-invasive, non-contact device to help doctors with their clinical judgment. As an example, consider a patient with necrotizing fasciitis or cellulitis, where a misdiagnosis for a patient like this can mean the difference between life and death. Thermographic testing helps clinicians to more accurately diagnose and treat these patients.
One of Aviles’ patients was in the postoperative phase of a complex knee procedure. In the visual assessment, there was no redness, so the patient’s doctor wasn’t concerned. However, Aviles’s imaging showed a positive 4.5, indicating abnormal inflammation. The patient had an infection inside the knee component that was so intense that he ended up with an above-the-knee amputation. His visual assessment never showed his infection, but thermography did.
Can thermography show lymphedema? No. Aviles says that although this type of test can’t positively confirm lymphedema, it’s still a helpful tool for clinical judgment.
Consider a study from South Korea on findings from using computed tomography on lymphedema, cellulitis, and generalized edema in lower leg swelling. Of 44 patients, 11 had cellulitis, 19 had lymphedema, and 14 had generalized edema. The moral of the story, Aviles says, is that patients with lymphedema have decreased oxygen to the tissues due to swelling and often end up with dermatitis or infections.
Swelling can also mimic what’s seen with ischemia. A patient with lymphedema might have ischemia-like symptoms, but testing shows good blood flow. Because of the distance from the skin to the capillary, oxygen is not getting to the skin. This is why a transcutaneous oxygen measurement calls for a challenge test to determine if inflammation and swelling could be the cause.
Aviles shares a case that hits close to home for him. His oldest daughter, Hannah, had her third ACL surgery, which was more complicated than the previous two. The doctor told Aviles that she was in the operating room much longer. They took the graft, the hamstring from the left knee, and put it on the right for the ACL. She had swelling visually, but on Aviles’ scale, she was borderline between being infected and not infected.
Aviles started treating his daughter with manual lymphatic drainage (MLD) to decrease the temperature. Within one month, she was showing slight inflammation, but the intensity of the thermographic imaging decreased.
Patients without fully functional lymphatic systems can’t decrease inflammation on their own. Aviles suggests that this could be tied to infections and explains that he and a group of colleagues are working on an article about post-operative total knee replacement patients where thermography is helping address their edema.
The examples above show how thermography detects the temperature or radiation emitted from the body, which can demonstrate that there is abnormal inflammation. This allows healthcare professionals to address patients’ needs much more quickly.
Further Examples
Aviles shares that he has many examples of the differences between visual examination and thermographic imaging. One of his patients came in with an infection in his leg. The patient was treated in the hospital without antibiotics. On the last day, when the patient was packed and ready to go home, Aviles’s input was requested.
Visually, the redness stopped at the midfoot, but the patient’s scan showed that the redness underneath the skin went all the way up to the knee. Based on this, Aviles suggested that the patient should not go home and advised that if he went home, he’d likely return the next day.
As Aviles predicted, the patient was back at the hospital the next day. His infection was worse with increased pain, and he ended up losing part of his foot. The situation is a reminder that abnormality often extends far beyond the skin. Aviles notes that if the patient had darker skin, his dire situation might have been even less noticeable from a visual inspection alone.
In another instance, Aviles saw a patient who was frustrated about not making progress with his condition. The wound was only 2.1 centimeters deep but was red and neither regressing nor progressing.
When a wound is following this trajectory, there would typically be more granulation, which indicates the formation of new blood vessels. It shouldn’t be inflamed. In this case, the wound was initially viewed as a pressure injury, but the scan showed otherwise and revealed a 6.5-centimeter tract.
This patient, who would have been headed to an outpatient clinic, was now headed for surgery. Aviles reflects on the experience and says that although this patient might have eventually shown signs of an infection, scanning allowed a deeper look to catch it early.
In general, thermography allows much earlier prediction of which wounds may open. Aviles says it’s possible approximately 30 to 41 days before it happens but cautions that there is a known false positive rate. Long-wave infrared thermography doesn’t have 100% accuracy, but there are promising results.
About Lympha Press
This informational webinar about infrared thermography for lymphedema and wound care was presented by Lympha Press, which provides at-home pneumatic compression therapy options with results backed by clinical studies. Visit the Lympha Press site to learn more about how Lympha Press can help your patients with chronic wounds.