This is a 14-minute read.
Lympha Press was honored to, once again, feature Dr. Karen Herbst as a webinar speaker sharing the latest in lipedema research and practice. Dr. Herbst is a prominent figure in lipedema research and the Chief Medical Officer at Lympha Press, where she has been a leader in supporting and encouraging advances in lipedema care with our organization.
In this particular webinar, Dr. Herbst presented the science behind, and potential applications of, a new theory regarding the relationship between subclinical compartment syndrome and lipedema. Specifically, her theory purports that, in some cases, subclinical compartment syndrome may influence the pathophysiology of lipedema. Dr. Herbst acknowledges the important contributions of her colleague, Dr. José Luis Simarro, whose expertise helped to shape much of the information and developments discussed. Here we will review some of the key components and take-home messages of this innovative theory, as well as let you know where you can find more information about it.
4 Foundational Concepts of Lipedema
While many may be familiar with the lipedema condition, Dr. Herbst reminded us that it is a disorder involving fat tissue. It most commonly occurs in women and presents in the thighs, arms, torso, and abdomen, while hands and feet are typically unaffected. Many patients experience tenderness or may bruise easily in the affected areas. She pointed out that these features of the condition are due to four well-researched concepts:
- There is an immune response component to lipedema – Increased levels of platelet factor four, macrophages, cytokines, inflammatory angiogenesis (or blood vessel growth), and microangiopathy (inflamed vessels) support that the immune system is activated in lipedema tissues.
- Lipedema tissue is metabolically unhealthy – While there is still research needed to understand why, scientists and physicians do know that one of the ways lipedema grows is by expanding existing adipocytes (fat cells). The presence of hypertrophic adipocytes has a strong relationship with insulin resistance and other metabolic markers indicating that they are unhealthy.
- The venous system is impacted by lipedema – Approximately 25-50% of women with lipedema also present with varying forms of venous system issues (e.g., chronic venous insufficiency, varicose, or reticular veins) but we have little research to fully understand why this may be.
- There is no lymphatic obstruction in women with lipedema – Though imaging has confirmed that impaired lymphatic vessels may be leaky, sluggish, or dilated, we can confidently say that lipedema shows no obstruction to the system. We also know that malfunctioning lymphatic vessels (as seen in lipedema) can contribute to fat growth.
Altogether, each of the components of lipedema (i.e., having an inflammatory immune response, unhealthy tissue, and venous and lymphatic insufficiencies) can stimulate fat growth.
What Are Muscle Compartments and Compartment Syndrome?
Though lipedema tissue growth concepts have been firmly established in lipedema literature, Dr. Herbst highlights that there has been little to no research on how these fat growth stimulants relate to muscle compartments in our limbs. Compartments are bundles of muscle, nerves, blood vessels, lymphatic vessels, and adipose tissue surrounded by fascia that exist in the arms and legs. Compartment syndrome occurs when there is increased pressure within the compartment, leading to pain and tissue damage. Dr. Herbst notes that this increased pressure can be caused by swelling from injury or an overgrowth of tissues, leaky lymphatic or blood vessels, or shrinking and hardening of the surrounding fascia over time.
Lipedema Pathologies and the Saphenous Compartment of the Leg
After giving the audience an overview of the two major conditions discussed in this theory, Dr. Herbst helped to connect the dots on how lipedema pathologies may be related to subclinical compartment syndrome. She went on to identify three adipose compartments in the leg: superficial, deep, and saphenous. The saphenous compartment is a small compartment of the inner leg, home to the greater and small saphenous veins, that receives drained fluids (blood and lymph) from tissues both within and outside of this compartment. Dr. Herbst also noted that the location of the saphenous compartment on the inner thigh and calf also mirrors where we typically see fat overgrowth in patients with lipedema.
To help drain blood out of this compartment and back to the heart, the saphenous veins indirectly rely on the calf muscle contractions which compress large deep veins that, in turn, compress the small superficial saphenous veins. However, if excess adipose tissue is present (as seen in lipedema) then the tissues and fibrotic surrounding fascia are unable to adequately compress and flush out the fluid. This impaired pump process can then cause a reflux of lymph into the saphenous compartment space.
This is a major point in Dr. Herbst’s new theory. She highlighted that the excess tissue, leaky or sluggish vessels, and stagnant interstitial fluids lead to further inflammation within the saphenous compartment and mirror known lipedema pathologies. Therefore, these conditions may encourage additional fat tissue growth (lipedema), inhibit superficial lymphatic system function, and lead to increased compartment pressure.
To further support this theory, Dr. Herbst pointed out that the foot is often unaffected by lipedema. The foot is the only location where the deep lymphatic can adequately clear the lymph fluid even if the superficial system fails. In contrast, the upper calf and thigh, which are common lipedema locations, rely on both the deep and superficial systems. However, if the superficial system fails, Dr. Herbst noted that the deep lymphatic system cannot completely drain the thigh and calf areas. Those tissues rely on fluid being removed via an alternate route, a recently identified interstitial organ (interstitium) discovered in 2018.
The interstitium is a network of fluid-filled spaces throughout the body’s connective tissues that link to the lymphatic system. Dr. Herbst suggested that when deep and superficial lymphatic vessels fall short, excess fluid is drained to other parts of the body through these interconnected, interstitial channels. This idea is supported by the common clinical practice of prescribing advanced pneumatic compression pumps to women with lipedema. The pump ensures that fluid from their lower limbs is thoroughly dispersed, rather than collecting in the pelvic and abdominal tissues and interstitial spaces immediately neighboring the affected areas.
Further Evidence to Support This Theory
In addition to the theoretical reasoning supported by anatomy and physiology principles, Dr. Herbst shared imaging and clinical observations that further support the new theory.
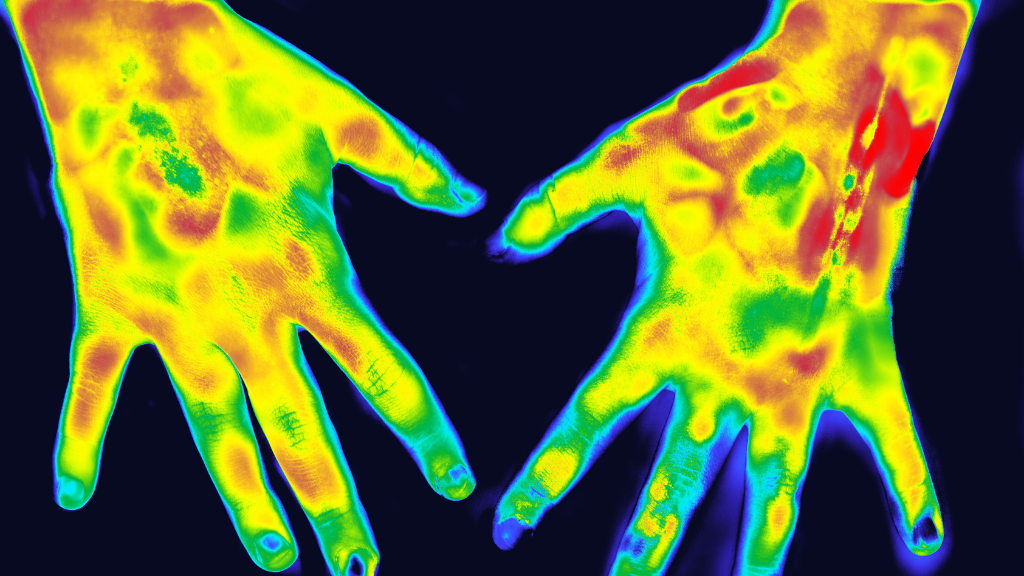
- In a transverse section of a leg from a woman with lipedema, there was significantly more fat growth noted within the saphenous compartment compared to the other two leg compartments. Additionally, enlarged periphery veins were suggesting that there may have been increased compartment pressure.
- In ultrasound imaging, you can easily see fibrotic deep fat within the compartment and near the saphenous vein. This fibrotic tissue could create contracted and inflexible fascia surrounding the compartment. As described above, these changes in fascia could in turn lead to the compressing of the internal tissues, impairing the normal flow of venous and lymphatic fluid for saphenous compartment output.
- After sharing imaging findings, Dr. Herbst again noted the role that inflammatory sources play in triggering lipedema and fat growth. She even reminded us of the high prevalence of hypermobile joints in patients with lipedema and hypothesized that repetitive microtears in joint tissues acted as triggers. The effects of these microtears could initiate or exacerbate fat growth and somewhat mirror the studied chronic, exercise-related compartment syndrome in athletes.
- Many women report tenderness and pain in areas of lipedema. This further supports the theory of related compartment syndrome development as pain and tenderness to touch are also hallmark signs of this condition. Dr. Herbst suggested that perhaps the discomfort these women are feeling is related to underlying, undiagnosed compartment syndrome.
Overall, Dr. Herbst laid out the similarities and relationships between lipedema and compartment syndrome pathologies suggesting a connection between the two conditions.
Diagnosing and Treating Compartment Syndrome in Lipedema Patients
Dr. Herbst also spent time unpacking suggestions for the next steps, including diagnosis and treatment of compartment syndrome in lipedema. She reviewed examples in the literature of doctors using a diagnostic device to measure the muscle compartment pressure before and after exertion. Dr. Herbst reported that while this method of compartment syndrome diagnosis has likely never been used for lipedema, it could be adapted for patients with lipedema given the similarities in presentation between both conditions.
Potential treatment options she shared included some of the following interventions and approaches:
- Anti-inflammatory approaches commonly used in lipedema care could also support compartment syndrome management, such as diet, exercise, supplements, or medications.
- Lipedema reduction surgery may also support compartment syndrome by alleviating pressure for comfort and muscle pump functioning for fluid drainage.
- Stretching regimens may help to maintain soft tissue pliability to prevent fibrotic fascia and maintain compartment flexibility.
- Orthotics, bracing, or strengthening exercises may help to correct maladaptive posture commonly seen with lipedema and support individuals with hypermobility by reducing micro-tearing and inflammation of joint tissues.
- Vascular interventions have the potential to support lipedema and compartment syndrome conditions by supporting healthy venous drainage and subsequently reducing inflammation.
Although these are long-established treatment approaches, this new theory highlights a potential for new applications. These evidence-based interventions may help to address the known and suspected underlying pathologies of lipedema and compartment syndrome.
Dr. Herbst Shares More of Her Lipedema Expertise
After presenting the new theory, Dr. Herbst addressed questions from the audience. Questions sought to further understand this theory, explore additional applications of the theory, and understand broader concepts in lipedema. Here is a sample of the topics covered in the Q&A with Dr. Herbst:
- Does compartment syndrome present symmetrically?
- Is there a relationship between livedo reticularis and lipedema?
- Does diuretic medication help or hurt lipedema pathology and symptomology?
- Are there lipedema treatment precautions one should consider while managing comorbid inflammatory diseases (i.e., could manual lymph drainage exacerbate Lyme’s disease symptoms)?
- Is there a correlation between conditions of elastin deficiency, such as Williams syndrome, and the development of lipedema?
- What treatment tools are best for targeting deep tissue treatment in lipedema?
- How can lipedema patients best advocate for themselves while working with medical professionals to explore possible compartment syndrome?
- Should statin drug use to stabilize blood vessels be considered a therapeutic approach for lipedema?
These questions and several more were answered to help the audience better understand the presentation and treatment of lipedema and compartment syndrome. If you would like to hear Dr. Herbst’s responses to these questions, the webinar can be viewed here (Q&A begins at 49:00). A key takeaway from the Q&A session was that knowing more about the signs, symptoms, and potential treatment approaches of lipedema and compartment syndrome allows patients and healthcare providers to better advocate for optimal care.
A New Look at Lipedema: “A Disease of Compartments and Their Contents”
As Dr. Herbst summarized, this new theory offers a new lens for viewing lipedema “as a disease of compartments and their contents and not just fat tissue.” The hypothesized relationship between lipedema and compartment syndrome has the potential to enhance and advance lipedema care and quality of life for patients. It offers providers an innovative way to think about how they consider, diagnose, and treat the conditions. We appreciate Dr. Herbst’s willingness to speak with us and share her experience.
If you were unable to attend our live event, or simply want to rewatch and review this topic, you can view the webinar recording here. We also invite you to explore our additional resources for more on lipedema care and research.